by Nesrin Abu Ata | Sep 27, 2022 | Mind Body Medicine Sioux City
QUESTION FROM A READER: I noticed that my daughter, who is 14 years old, always wants to wear long sleeve shirts and wants to cover her wrists. The other day, I saw scars on both of her wrists and inner thighs. She talks about how other girls in school cut on...

by myklroventine | Sep 11, 2022 | Mind Body Medicine Sioux City
Originally published on #SameHere Psych, samehereglobal.org

by Nesrin Abu Ata | Aug 17, 2022 | Mind Body Medicine Sioux City
A QUESTION FOR THE DOCTOR: Dr. A, My 12-year-old daughter struggled with being overweight until she hit a growth spurt. Her weight stayed the same but she grew a few inches. Nobody has ever said anything about her weight, but she recently became obsessed with her...

by Nesrin Abu Ata | Aug 3, 2022 | Mind Body Medicine Sioux City
QUESTION FROM A READER: My tween spends most of her time on her smartphone. She has no interest in hanging out with us as her family. Even when she is sitting with us, she is constantly scrolling through her phone, and doesn’t engage with us. When we take her phone so...

by Nesrin Abu Ata | Apr 19, 2022 | Mind Body Medicine Sioux City
QUESTION FROM A READER: I have been struggling with my sleep lately and wondering about natural ways to help me with my sleep. Because I haven’t been sleeping well, I am tired during the day. I have tried over the counter medications, but I have woken up with a hang...

by Nesrin Abu Ata | Dec 4, 2021 | Mind Body Medicine Sioux City
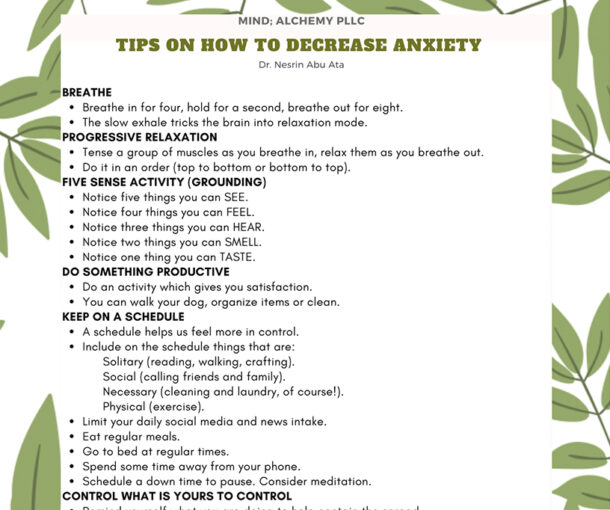
QUESTION FROM A READER: I have been diagnosed with an anxiety disorder and I am interested in holistic tools and more natural medicines to manage my anxiety. What treatment options should I bring up with my mental health provider for my treatment for anxiety? ANSWER:...